Perimenopause: Everything You Need to Know
After 6 months of research and personal experience, I have compiled all the most important information for you to know.
I’m not a doctor. Let’s start there.
Nothing I am about to share should be considered medical advice. Don’t worry, I will share really great resources with you, from doctors to follow to websites to visit and books to read. They are the resources for this article and they are amazing.
What this is, is a 4500+ word dissertation I’ve put together so that you, any person born with female reproductive organs, will know what happens in the perimenopause stage of life and be able to do something about it.
Because, my friends, it’s a lot.
About 6 months ago, I found myself feeling an overwhelming, all-encompassing rage brought on by not being able to get one of my sleeves to lay correctly on my arm. Truly. It’s embarrassing how angry I was; I wanted to grab the sleeve and viciously rip it off of the shirt. That’s how intense and utterly disproportionate my feeling of rage was.
I had to pause. I knew that this was not OK and I also knew that this was more than PMS.
I was livid.
On the other side of things, I was also crying. A lot. I didn’t know if it was grief (I was dealing with something major) or depression. Maybe both? Maybe neither?
One time I was curled up in a ball on my bed, crying so hard I was shaking. And I couldn’t identify a reason why.
To be honest, it scared me.
My third big emotional symptom (I’ll talk about the physical symptoms later in this post), was this feeling of “who fucking cares” about almost everything in my life.
I felt no motivation to do anything, both in my personal life and in my work. I was ready to just walk away from it all.
I can’t even remember how I came across the word “perimenopause”. I was probably still reeling from that shirt situation and looking for a chat room of others who have mutilated their own clothing out of sheer rage. I didn’t find one.
What I did find was the word “perimenopause”. And from that moment on, I felt so freaking validated and understood that I (can you guess?) — cried.
But this time it was tears of joy.
Joy at finally knowing that I was not losing my mind, I was not depressed, and I was not alone.
As my research continued, I started to share some of what I was learning with friends of a similar age to me — late thirties to late forties.
The first thing I shared was that “menopause” is actually just one day— the day that marks one year since your last period or, a more accurate definition according to Dr. Mary Claire Haver, is the day we no longer have any eggs left and therefore very little sex hormones produced from the ovaries- and everything leading to that date, it could be up to 10 years before that date, is called perimenopause.
Every single one of my friends was surprised. No one knew this.
This made me go 🤨.
We all just thought of menopause as the hot flashes that we see in sitcoms and movies. And this is simply not the case.
What is the case is that there is a very long list of symptoms brought on by the loss of estrogen and that this loss can lead to significant health problems later in life if not addressed.
According to Dr. Mary Claire Haver, an OBGYN and menopause specialist, while women tend to live longer, our quality of life in the final 10 years tends to be much less than men, and researchers are discovering now that the loss of hormones is a very big part of that.
I assume we’re all on the same page in terms of wanting to still be able to hover over public toilets when we’re in our eighties? 😬
Cool.
via @estogen_matters
That’s why I made it my mission to read 3 books, countless articles, watch at least 10 videos, listen to podcasts, and dig through countless Instagram posts from various experts in order to distill it down to what I think is the most important information to share with you.
Information that can arm you with the knowledge to speak to your doctor, or find one, who can help you navigate this very important, but also very misunderstood, time in our lives.
This excerpt from peri menopause power. said it best:
There is an intensity to perimenopause that we are rarely prepared for, but desperately need to be, because rather than it being something that happens to us, we can have a state of agency over our experience and find our power.
Like this Candidly article says, “…being informed is the very best way to prepare ourselves for every single sneaky stage of menopause. And the key to keeping ourselves happy/healthy through it all.”
So let’s dive in.
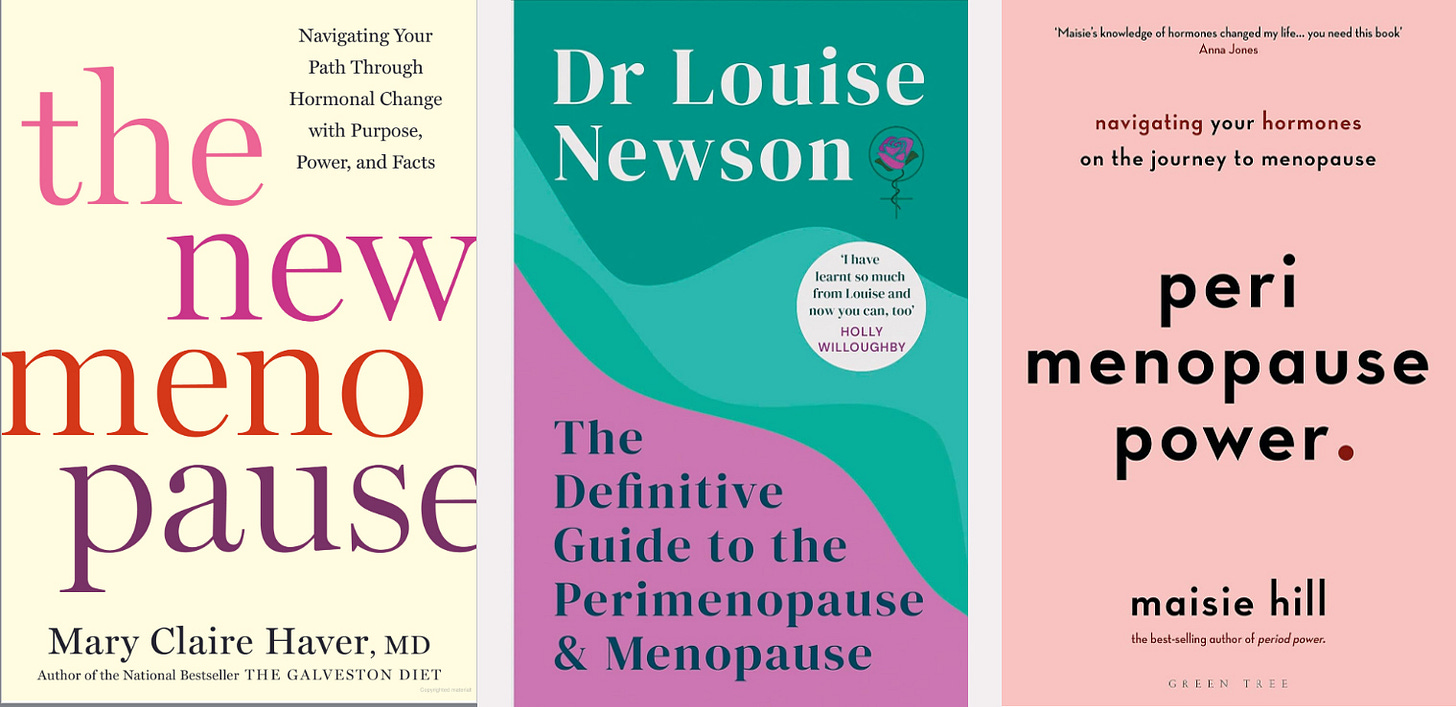
To begin, here are the three books I used in my research.
DATA AND STATISTICS
In an effort to make this post digestible and truly helpful, rather than going into every single detail of what I read, I will share data points and link to the articles, videos, and social media posts they come from so that you can dive into anything you’d like to learn more about.
Only 20 percent of doctor residencies offer menopause training.
Medical students specializing as OBGYNs receive little to no training on menopause. Read that again.
Consider the impact of this when we, women entering into perimenopause, visit our doctors with a list of symptoms and a lot of questions and they really have minimal idea how to help.
It is incredibly common to be completely dismissed or misdiagnosed during these visits. All three books I read share true accounts of women struggling to get help because their doctors don’t have enough education about menopause.
In 2021, the National Institutes of Health reported that $5 billion in federal funds would go towards women’s health. However, only .003 percent will go towards menopause research.
According to Dr. Mary Claire Haver, “by the year 2030, the world population of menopausal and postmenopausal women is projected to increase to 1.2 billion, with 47 million new entrants each year. Can you imagine the power of a population this size if we can unite to demand continued improvements in the standard of care for women at this stage of our lives?”
“As your body produces less estrogen….your risks for developing serious medical conditions - including diabetes, dementia, Alzheimer’s, osteoporosis, and cardiovascular disease- go up.” - The New Menopause
A study published in the journal Menopause reported that a woman starting estrogen at fifty can expect to live up to two years longer than women who don’t.
“The dip in estrogen during the menopause transition literally changes the female brain.”- based on a study by Dr. Lisa Masconi
A central feature of menopause is the decline in the body’s production of estrogens. This leads to various bodily changes including the cessation of menstruation, but also to neuropsychiatric effects such as “brain fog,” depression and anxiety.- Weill Cornell Medicine Study
1 in 5 women will quit their jobs because of menopause symptoms. -Dr. Haver.
Women are living longer than men, but 20-25% of that life is in poor health. - Dr. Haver.
Yeah, holy shit.
SYMPTOMS LIST
In The New Menopause, Dr. Haver says: There are estrogen receptors throughout almost every organ system in your body [which means that every part of your body is used to functioning with estrogen], and as your levels drop, these cells begin to lose their ability to assist in maintaining your health in other areas, including your heart cognitive function, bone integrity, and blood sugar.
And when you think about that, you likely won’t be surprised by the long list symptoms that 30-50% of women experience that impacts their quality of life.
Sounds fun, huh?!
I also loved this skit that shows some of the more bizarre & unsettling menopause symptoms. I have totally felt the sensation of bugs crawling on me as a symptom!
Now, if you find the medical side of things interesting, and weight gain has been one of your symptoms, you might want to watch this Instagram Live from Dr. Newson. I found it fascinating but if the medical side of things doesn’t interest you, maybe skip it.
Anyway, is this not the most intense list of symptoms you’ve ever seen?
If you identify with some of these symptoms, it is worth talking to your doctor about whether you could be in perimenopause.
According to Dr. Newson in The Definitive Guide to the Perimenopause and Menopause, “as a general rule, the perimenopause begins in the early to mid forties- though it can happen later or much earlier for reasons including genetics or due to surgery or treatment.”
Something important to note, the average age of menopause in American women is 51, which means that many women hit menopause as young as 45 and perimenopause as young as 35.
Listen to this:
Meaning this post isn’t just for my 40+ ladies. If you’re in your mid to late thirties, you should keep reading too.
Honestly, no matter what age you are, YOU NEED TO KNOW THIS STUFF!
I hope you’re learning a lot reading this post. I write without a paywall, but writing does take time. If you enjoyed this post, I’d be honored if you bought me a coffee — it fuels my writing! Thanks, friends.❤️
HRT (ALSO KNOWN AS MHT)
I know there has been a lot said about hormone replacement therapy or menopausal hormone therapy over the years.
Back in 1998, the Women’s Health Initiative launched a study on menopausal hormone therapy and what happened with this study had a massive impact on women’s health, not for the positive.
So let’s get a snapshot of what this study did.
It studied post-menopausal women (they were in their 60s) with a focus on prevention of chronic diseases through hormone therapy (estrogen and progestin).
I won’t go into all the tiny details (read any one of the 3 books I shared to get get a much better understanding of what it was all about) but suffice it to say that what was supposed to be an 8.5 year study was abruptly stopped in 2002 because there was found to be a slight increase in breast cancer risk found in some of these women.
There was also a decrease in colon cancer and osteoporosis found. But these things got lost in the uproar about the breast cancer increase.
Once this came out, a massive percentage of women who were on hormone therapy stopped receiving it and very few women were offered it moving forward.
According to The New Menopause, “all the public got at the time was drama in the form of inaccurate reporting and alarming headlines that was reduced to: estrogen causes cancer.”
Here’s what’s important to know about the “risk” of breast cancer from estrogen, as clarified by Dr. Haver:
In the WHI study, the chance that a woman would develop breast cancer was four out of one thousand per year on placebo. When estrogen and progestin were added, that risk increased to five out of one thousand women per year. That increased risk is 0.08 percent.
I’m not telling you to go in hormones. I’m just telling you about the actuality of this study so that you aren’t holding on to false research outcomes perpetuated by the media and scaring you into completely disregarding a treatment that could be a life-changing option for you. (It has been for me).
Let’s look at what studies are now saying about hormone therapy.
Studies show that women who are given hormone therapy in their perimenopause have a lower incidence of depression.
Studies show that hormone therapy lowers heart disease and heart attacks.
Studies show the hormone therapy protects the bones from weakening and breaking. (Side note, it’s astonishing how many people don’t survive long after breaking a hip in old age)
Studies show that hormone therapy lowers the risk of type 2 diabetes
Studies show that hormone therapy decreases your risk of death from any cause. Meaning, if you’re diagnosed with something, you have a better chance of beating it when you’re on hormone therapy.
Studies show that the earlier a woman starts hormone therapy, the better her future health.
Some people say hormone therapy is over-medicalized. I suggest watching this clip from Dr. Haver for a different perspective. Only 6% of women in the US who are eligible for hormone therapy are receiving it!
The other thing to know about hormone therapy is there really isn’t a test to determine what your hormones are doing. Because hormone levels can change through a single day, a blood test isn’t an accurate representation of your levels.
Instead, doctors who understand menopause tend to ask your symptoms, do tests to rule out other health issues, and then if all are negative, talk to you about perimenopause and menopause. The knowledgeable ones will tell you about your hormone therapy options.
The ones lacking knowledge will tell you that “you're aging, so exercise more, eat less, and toughen up”, in so many words. (This is when I expel a very frustrated sigh).
Anyway, when considering hormone therapy, you want to do your research before going to see your doctor (more on this below). But make sure to look into the types of hormone therapy (bio-identical vs synthetic, patch vs pill vs cream vs vaginal insert, etc.). Get one of the books I mentioned and deep dive into the section on Hormone Therapy.
Like I said, I’m not a doctor and I want t be careful of how much I write about HRT in this article. So I will just say, if you see yourself in those symptoms and you want relief, do yourself a favor and discuss hormone therapy with a doctor who gets it.
NUTRITION + EXCERCISE
MHT alone is not enough to minimize the symptoms and improve our health during perimenopause and menopause.
I have found that making changes to my nutrition and exercise routines, in addition to taking hormones, has made a huge difference in my symptoms and my overall feeling of wellbeing.
Click on the below slideshow, it’s helpful.
I was blown away when I learned about the difference between subcutaneous fat and visceral fat. Visceral fat is the fat that wraps around our organs and is a harbinger of chronic disease.
Subcutaneous fat is what we see, it stresses people out because society has told us it isn’t “attractive”, but it doesn’t bring the risks that visceral fat bring.
8% of our fat is visceral fat when we are pre-menopausal, it goes up to 23% when we are perimenopausal. -Dr. Haver
We’ve all heard how important physical activity is for our health. And as we age, it’s not uncommon for the type of exercise we do to change in order to better suit the changes our bodies are experiencing.
Up until recently, the “cardio queen” approach to exercise was all the rage and strength training was something too many women put out of their minds for fear of bulking up and not being “skinny”.
I get it. I used to go to barre class 3 or 4 times a week and I really enjoyed it. I had visions of ballerina body (to be clear, there is no exercise in the world that will give me ballerina body, since that is simply not my physical make up).
But as I got further into my forties, it was becoming clear that barre wasn’t enough. It wasn’t addressing my visceral fat and it wasn’t helping me build strength.
I wasn’t really seeing many benefits and as I started to get deeper into my perimenopause research, I realized that I needed a different approach.
According to The Menopause Society, “There are many physical activities that have been shown to help protect and strengthen the heart, bones, and muscles, as well as maintain and improve balance, body weight, mood, and one’s overall sense of well-being. You’ve got to mix it up a few times a week to keep improving your health. Here are a few activities to introduce variety into your routine:
Brisk walking
Jogging
Biking or spinning
Aerobics
Dancing
Tennis
Weight training
Interval training
I have adopted 3x per week brisk walks of roughly 4 miles in 1 hour (a 15 minute mile) plus 2-3x per week weight/strength training. I would love to introduce dance into the mix and will probably start taking salsa classes in the Fall!
I think for so long, we were trained to focus on burning calories. So hours spent on the peloton or running seemed to be the most important. It was always all about the cardio.
But that’s not enough.
It has to be a balance of cardio, strength training, and stretching.
With weight training, we should think about increasing resistance (I think this is where barre was falling flat for me).
Another piece of information from The Menopause Society states that, “As you get stronger, you must increase the amount of resistance you use to keep building strength. Your muscles should fatigue between 8 to 12 or 12 to 15 repetitions.”
I’m realizing as I write this that it’s time for me to up my weights, as I can do 15 reps without much fatigue.
With stretching, it’s important to build a habit of stretching every day because honestly, losing flexibility as we age just sucks.
I really like that Movement Living offers up free exercise classes each week that are on rotation based on a theme.
Since beginning my journey with perimenopause, I’ve learned to think about exercise and nutrition not to “getting skinny” but to get strong.
And in general, I’ve kept these things in mind in terms of my diet:
The more protein we consume, the less likely we are to be frail as we age. So eat a lot of protein throughout the day.
We start to process alcohol differently in perimenopause so I have started introducing non-alcoholic drinks into my social situations.
We need to make sure we’re getting enough vitamins like calcium, vitamin D, and iron. We should get as much as we can from food and then go with supplements to reach the recommended numbers if need be.
Fiber is a big deal, don’t ignore it.
I don’t like to think about things that I’m removing from my diet. I love food, almost all food, and I don’t intend to stop enjoying it.
Instead, I’ve approached it a few ways:
The 80/20 rule. Fridays and Saturdays tend to be days when my partner and I grab breakfast out or order a pizza and watch a movie, or make dinner reservations. And I love and revel in these times, guilt free.
Looking at my meal. By this I mean, whatever I have plated up for a meal at home, I see if there is anything I can add to boost it. Like, a hard boiled egg or a banana or berries or an avocado, or cottage cheese, whatever!
Probiotics. I have really been getting into gut health lately (more on that in another article) and I try to have a probiotic everyday. Sourdough bread (I’m very lucky to have a partner who makes incredible homemade sourdough regularly), Kombucha (another homemade treat from my partner), yogurt, kimchi, or even miso.
Curbing my sugar intake. I love ice cream. I’m doing my best to be more thoughtful about how often I enjoy it (and other sweets) but I’m not cutting sweets out completely because that would feel limiting. Luckily I love dark chocolate so a small piece of that usually helps with any sweets cravings.
I have started to think about my nutrition and exercise routine in the same way that I think about my money…
Invest in dividends now because it will multiply in the future.
This is where I remind you of the public toilet hovering goal!
Just remember that when it comes to exercise and nutrition, it’s not about being perfect. It’s about feeling strong, energized, and satiated, prioritizing your needs, and finding balance and enjoyment.
MENTAL HEALTH
Before I get into sharing how to find menopause specialists and other logistical things, there is one last area I want to cover. And that’s mental health.
I started this article with a story about my mental health. While I shared that story with a bit of humor, it is a true story that was actually really serious.
I didn’t know what was happening to me or why. I wondered if I was depressed, I wondered if the grief I had been experiencing was the cause.
I did not for one second think it was perimenopause. It never crossed my mind. It wasn’t until I stumbled on the word that I began to think it could be the answer.
Here are a few facts shared to Dr. Newson,
Feeling down, sad and upset can be very common symptoms of the menopause and perimenopause. Other psychological symptoms include feelings of low self-esteem, reduced motivation or interest in things, anxiety and panic attacks, irritability and mood swings.
Fluctuating hormones can have an immense impact on mental health. Previously rock-solid relationships can begin to falter, work may seem insurmountable, and activities you previously took pleasure in now feel like a chore.
Women are two to four times more likely to experience major depression during the perimenopausal or early post-menopausal phase.
Dr. Newson also shares this in her book: “…if you feel your moods have become more extreme…it is worth asking yourself the questions below to see if hormones are the are the cause.
Am I feeling more down/worried/irritable/angry than usual?
If you are still having periods, do these mood changes happen around my period?
Have these feelings become more intense?
Are my moods affecting my life in terms of motivation, sleep, eating, exercise?
Are these moods affecting work and home relationships- are these changes affecting those close to me more than usual?
Have these mood changes lasted foe a few weeks?”
If the majority of your answers is “yes”, talk to your doctor.
And as an important note, people can have two things. Mental health should be taken seriously; we cannot attribute everything to menopause. If you’re experiencing depression, talk to your doctor.
HOW TO FIND SPECIALISTS
Before finding your menopause specialist, it’s a great idea to create a daily symptoms log.
In your daily symptoms log, record everything you are experiencing — the common, the weird — all of it. And also the intensity.
I did this and created a 0-3 star scale so that every day I would list my symptoms in a note on my phone and add a number of stars next to each symptom.
I did this for almost two months while I waited for my appointment with my doctor.
As I mentioned, there is no test that can tell your doctor whether you’re perimenopausal. This log is so helpful in that regard.
Below is a list of resources for finding doctors who are menopause specialists.
I would like to point out that it is possible that your current doctor has taken it upon themselves to learn more about menopause health — I was pleasantly surprised when I visited my doctor that she immediately suggested that I’m in perimenopause based on my symptoms logs and had an open and honest conversation with me about hormone therapy.
I went in there armed with research and facts and ready to “fight” LOL. Luckily, I didn’t have to.
But you may have to. And you may decide that you don’t want to fight with your current doctor but instead see someone who gets it and gets you.
The North American Menopause Society: these are certified Menopause Practitioners
The Pause Life: started by Dr. Mary Claire Haver. These are vetted and recommended doctors
Gennev: menopause-trained doctors and registered dietitian nutritionists
Midi: clinicians specializing in menopause care
Menopause Care: Britain’s largest team of British Menopause Society accredited doctors and healthcare professionals
To continue your education, there are a lot of accounts you can follow on Instagram. I follow some but not all of these. I’m sharing this long list so you can choose the ones that you like.
I love following some of these accounts because these folks share so much knowledge, research, facts, insights, and information in short snippets that are easy to take in and then I research more on the topics that interest me.
I’m not suggesting following them all at once, but maybe save this post and come back to it every now and then to check out and add a few to your “following” list.
Doctors:
@jackiep_gynnp (Nurse Practitioner)
@showcenterdrq (Nurse Practitioner)
Communities:
Advocates:
Also, I highly recommend listening to this podcast episode: At the risk of causing a lot of eye rolls, I actually teared up listening to Dr. Haver in this Huberman Lab podcast episode. The combination of the infuriating data she shares and the passion with which she talks about what we as women deserve for our health and our lives is really, really moving.
I’ll leave you with this snippet of advice from Dr. Haver in the Candidly article about how to be proactive…
EDUCATE yourself and be prepared to advocate for yourself.
Maximize your nutrition - focus on high fiber foods, nuts, seeds, legumes, high quality protein (and make sure you are getting enough), avoid your personal triggers, keep added sugars less than 25g/day. Supplement gaps in nutrition as needed.
Exercise regularly - and not just cardio - strength training is critical to maintaining muscle mass, and therefore decreasing your risk of insulin resistance, diabetes, and visceral fat gain.
Reduce stress.
Prioritize sleep.
Consider pharmacology in the form of hormone therapy if you are a candidate.
*Some book links included in this post are affiliate links, which means that I get a couple bucks if you the buy the book using my link.
If you hit the ❤️ at the top or bottom of this post, you will not only make me very happy but you will make it easier for others to read Revel + Verve.
Your comments and hearts mean a lot. Thank you.











YOU'RE AWESOME!!
I'm literally bookmarking this article to my browser so I can find it quickly for references.
I'm about 2 years into perimenopause. When I first learned about it, about a year into this crazy roller coaster, the first thing that stuck in my head was "perimenopause can last up to 10 years!!" F*CK!!!! These 2 years have been the hardest mentally and physically in my life and I feel my body is just ramping up.
BUT with articles like this, a lot of research and literally rolling with the perimenopausal punches, I'm doing ok.
Thank you so much for so much information.
Thanks for such an informative post Nicole. I'll check out the books, and I'd also recommend The Menopause Brain by Lisa Mosconi, I learned loads from it.
TV presenter Davina McCall has done a lot of campaigning in the UK on menopause and gotten a lot of public discussion going which has been really welcome. I did our annual staff survey today (large organisation HQed in the UK) and I was pleasantly surprised to find there was actually a set of questions all about perimenopause experience!